With value-based care on the move in a major way, more and more healthcare providers are reorganizing their operations to meet new challenges. Success with value-based care requires providers to marry advanced technologies with people-powered strategies to get ahead of clinical and financial risks.
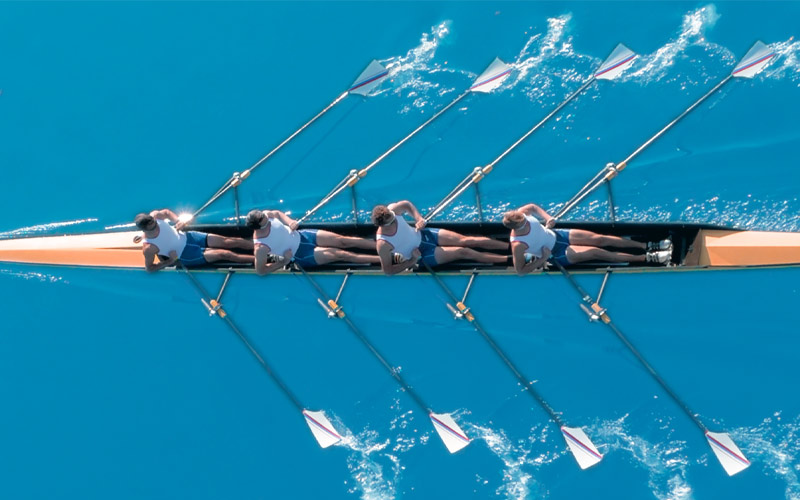
For many organizations, this means adopting a team-based care model that allows for the delivery of proactive, holistic services to patients.
While interdisciplinary care teams have the potential to maximize resources and improve experiences for patients and providers, they also come with challenges. Making sure that all members of the team are collaborating appropriately can be difficult, especially when digital information is delayed, incorrect, or incomplete.
As healthcare organizations transition to team-based care, they will need to develop strategies to serve up precise, meaningful, and actionable data to the right members of their care teams at the right time.
Why are care teams important for value-based care?
A care team is a group of clinical and non-clinical staff members, typically from complementary disciplines, who collaborate to manage the health of patients in a comprehensive manner. Clinical care teams typically include a physician, nurse practitioner or physician assistant, registered nurse, and medical assistant, each of whom takes on a different part of the patient care process.
For providers participating in value-based care arrangements, especially in the primary care environment, the care team is often extended further to address additional needs, including the social determinants of health. Social workers, care managers, health coaches, behavioral health providers, physical therapists, nutritionists, and other types of experts may all be involved in identifying and reducing risks for individuals and populations.
Team-based care allows each member of the team to operate at the top of his or her license while encouraging problem solving and appropriate hand-offs between professionals with different experiences and knowledge bases.
Both patients and providers benefit from this approach. Data compiled by the National Nurse-Led Consortium shows a 50 percent increase in patient satisfaction under team-based care – and equally important, a 43 percent increase in job satisfaction among staff members working in teams.
Well-designed teams also showed a reduction in medical errors, improved clinical metrics for patients, and better patient adherence to care plans.
Acknowledging the challenges of collaboration
Team-based care has clear benefits, but it can also create some problems if organizations don’t pay special attention to the health information that fuels collaboration. Miscommunication is a top culprit in medical errors and poor patient experiences. Avoiding mistakes and fostering an open, informed environment is key.
Each team member will view and generate his or her own data when interacting with an individual. They will also need to access insights from across the care continuum, including data created by payers, hospitals, labs, specialists, and even their own accountable care organization (ACO).
Without a way to easily identify changes to patient charts, synthesize the new data with existing information, and present the up-to-date record in a clear and precise manner, teams can quickly get confused and begin to collapse.
Team members working on population health management projects also have unique requirements. They need to access cohort-level insights while being able to drill down to the individual level in order to target interventions to at-risk individuals, conduct outreach, and follow up as needed.
With traditional technologies, it isn’t always easy for organizations to develop workflows that can empower care teams to work together efficiently and effectively for the good of the patient.
To create a data-rich environment that encourages seamless teamwork, providers will need to enhance their existing tools with knowledge delivery capabilities specifically designed to enable value-based care.
Using precision data to activate value-based care teams
Care teams are designed to reduce cognitive burdens, overcome barriers to care, and simplify operations. The technology to support team-based care should do the same.
Workflows that leverage automated sensors to identify new additions to a chart and surface relevant data in a contextualized way can further the positive impacts of the team structure. Magnifying this approach to include population-level insights can help providers meet their quality goals.
For example, Nancy, a care manager, is conducting her regular assessment of patients who may be eligible for a diabetes management program. She opens up her population health dashboard and reviews a real-time, dynamic list of patients with recent ED visits, out-of-range lab results, and upcoming A1C checks.
She notices that Mr. Jones has joined the list of at-risk individuals. Nancy drills down to his individual information and finds some lab results that are extremely concerning. Mr. Jones has a visit scheduled soon with Dr. Singh for a different health question, and Nancy wants to make sure that his physician discusses his rising risks for diabetes during the visit.
Under a traditional structure, Nancy might leave a post-it note for Dr. Singh reminding him to click through a few screens to the lab results in Mr. Jones’s chart. The doctor may or may not remember to do so and could miss the fact that Mr. Jones should be given a referral to a diabetes specialist. If this gap in care is not closed quickly, Mr. Jones could end up in the emergency department.
But with the right digital tools in place, neither Nancy nor Dr. Singh have to worry about missing anything. When Dr. Singh opens Mr. Jones’s chart, the new lab results are right there in the patient information ribbon at the top of his screen.
The automated, intelligent system has already used the red-flag data to initiate a referral to an endocrinologist and request authorization from the health plan. All Dr. Singh has to do is sign off on the action, saving him time and effort.
The next time Dr. Singh, Nancy, or any other member of the care team opens the chart, they will see that Mr. Jones visited the endocrinologist and started on a personalized care plan to get his risks under control.
All members of Mr. Jones’ team stay informed about what has happened and can help to keep the patient on track by enrolling him in a diabetes management program with a nurse practitioner and assigning him a social worker to help with a food insecurity issue. Mr. Jones will get better care, and Dr. Singh’s team is one step closer to meeting its quality and spending goals.
Combining smart technology with effective care teams can create a collaborative, informed, and activated ecosystem that proactively meets patient needs and helps providers reach their targets.
With greater automation and the precise delivery of information when and where it’s needed, healthcare providers can architect highly efficient and effective care teams that achieve the goals of value-based care.